What are Movement Disorders?
Movement disorders in children can present across a wide range of neurological conditions, from benign, self-limiting transient phenomena to progressive disorders that cause significant motor impairment. Clinical presentations may be acute, subacute, or chronic.
What Are the Types of Movement Disorders?
Movement Disorders can be divided into:
- Hyperkinesia (too much movement) or Dyskinesia (abnormal movement)
e.g. tics, dystonia, myoclonus, chorea, athetosis, tremor and stereotypies - Hypokinesia-rigid syndrome (too little or lack of movement)
e.g. Parkinsonism, which is rather rare in children
What are the Movement Disorders Presenting in Childhood?
1. BENIGN MOVEMENT DISORDERS OF CHILDHOOD
A number of benign movement disorders of childhood are recognised, and they are transient in nature, and usually have a good long-term prognosis.
Neonatal Jitteriness
- High frequency and low amplitude tremor
- Location: jaw and extremities
- Multiple factors, including metabolic disturbance, Hypoxic-Ischaemic Encephalopathy (HIE), drug withdrawal
- Often mistaken for neonatal seizures
- Suppressed easily by gentle restraint
- No specific treatment; treat the underlying factors
- Usually resolves by 7 months
- Usually resolves by 7 months
Benign Neonatal Sleep Myoclonus
- Self-limiting disorder
- Myoclonic jerks during non-rapid eye movement (NREM)/ quiet sleep
- Stopped by arousal; Usually resolves by 3 to 4 months
Benign Polymorphous Movement Disorders of Infancy (BPMDI)
A diverse group of movement disorders includes shuddering attacks, benign myoclonus of early infancy, head nodding, benign infantile shaking body attacks, brief tonic contractions, benign non-epileptic infantile spasms, and sleep-related infantile tremor.
Characteristic features:
- Onset: 4 to 7 months
- Paroxysmal, sometimes in clusters
- Brief event without impaired consciousness
- Several times on a daily basis
- Usually triggered by excitement, frustration or postural changes
- Normal developmental milestones, and normal neurology
- Resolved spontaneously
Transient idiopathic dystonia of infancy
- Onset is usually before 5 months
- Hemidystonia – usually affecting single upper limb and trunk
- Movement stopped when infant moves purposefully
- Resolves without any complications around 1 year of age
Motor Stereotypies/ Stereotypic Movement Disorder
- Repetitive, seemingly driven, purposeless motor behaviour
- Early onset
- Usually persists more than 4 weeks
- May interfere with normal activities, or results in self injury
Primary Motor Stereotypies
- Common among normal children
- Transient in nature; Good prognosis
- Common Behavioural stereotypies, such as rocking, head banging, hair twisting, pencil tapping
- Complex stereotypies: head nodding, hand shaking, opening/ closing of hands, arm flapping, flexion/ extension of wrists, mouth opening/ facial grimaces
Secondary Motor Stereotypies
- Frequently seen in children with Autistic Spectrum Disorders, Rett syndrome, Angleman Sydnrome, Neurogenetic disorders and Neurometabolic disorders.
2. TICS & TOURETTE SYNDROME
Please click Tics & Tourette Syndrome (妥瑞症) for further details.
3. DYSTONIA
Dystonia is characterised by sustained or intermittent muscle contractions that cause abnormal, often repetitive, movements, postures, or both. It is typically patterned and twisting and may be tremulous. It is usually initiated or worsened by voluntary action and is associated with overflow muscle activation.
Causes of childhood dystonia:
- Primary Dystonia, e.g. Dopa-Responsive Dystonia, DYT1-mutation.
- Secondary Dystonia, eg. Cerebral Palsy, Metabolic Disorders
What Causes Movement Disorders?
Our brain cells communicate with each other through electrical signals, which are facilitated by special chemicals called neurotransmitters. Movement disorders occur when there is a disturbance or imbalance of these neurotransmitters or when there are structural abnormalities in the areas of the brain such as basal ganglia, which are responsible for controlling movement.
Movement disorders can be caused by or associated with various factors, including structural, metabolic, infectious, immunological, or genetic and inherited conditions. It may also result from a combination of these factors or be idiopathic, meaning there is no known cause.
For example:
- Structural cause – Acquired brain injury, Cerebral Palsy (CP)
- Metabolic cause – Lech-Nyhan Disease causing generalised dystonia
- Immunological cause – Anti-NMDAR antibodies encephalitis
- Genetic cause – e.g. GNAO1 mutation related movement disorder
What Are The Common Co-Occurring Conditions?
Children with movement disorders may experience a variety of co-occurring conditions that can impact their overall health and well-being. Some common co-occurring conditions include:
Neurodevelopmental Disorders & Learning Disability
Children with movement disorders can experience mild, moderate, or severe learning disabilities. Current research indicates that the underlying causes of these movement disorders may affect neurodevelopment. Example: Rett syndrome.
As a result, children and young people with movement disorders are also at risk for neurodevelopmental disorders, which may include Attention Deficit Hyperactivity Disorder (ADHD), autistic spectrum disorder (ASD), and Obsessive-Compulsive Disorder (OCD).
Epilepsy and Epileptic Seizures
Some children with movement disorders may experience epileptic seizures. These seizures can vary in type and severity and may require treatment with anti-seizure medications. Example: SLC2A1 mutation disorders, GNAO1 mutation disorders.
Sleep Disorders
Sleep disturbances, such as sleep apnea, insomnia, and disrupted sleep hygiene, are more prevalent in children with movement disorders, affecting up to 30% of them. These disturbances can significantly impact overall health and quality of life.
Gastrointestinal Issues
Gastrointestinal issues, including gastroesophageal reflux disease (GERD), constipation, difficulty swallowing, and excessive salivary drooling, are common in children with generalised dystonia and other movement disorders. Proper management and dietary changes may be necessary to address these problems.
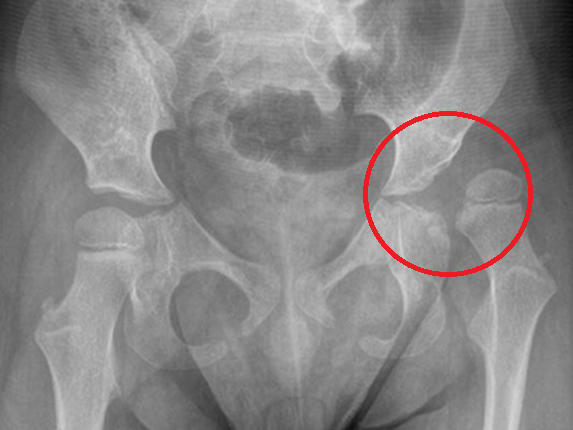
Orthopaedic Complications
Up to 30% of children with long-term neurological conditions, such as dystonia, are complicated by significant functional musculoskeletal impairment. These can manifest as hip subluxation (partial dislocation) or dislocation, scoliosis (twisting of the spine), and joint deformities, all stemming from muscle stiffness (due to dystonia or spasticity) or muscle weakness. Addressing these serious complications is crucial.
Effective management often requires a multi-faceted approach, incorporating physical therapy, targeted medications, orthotic devices, or even surgical interventions, such as Deep Brain Stimulation (DBS) or Intrathecal infusion therapy . Prompt and comprehensive treatment can make a profound difference in these children’s quality of life and overall mobility.
Sensory problems (Visual & Hearing problems)
Depending on the cause of the movement disorders, visual impairments, which may include squint (lazy eyes), nystagmus (involuntary eye movements), or cortical visual impairment. Regular ophthalmological assessment and interventions may be necessary.
Children with movement disorders may also experience hearing impairments, either due to congenital factors, complications of prematurity, or repeated ear infections. Hearing assessment and appropriate interventions are essential for optimal communication and development.
Behavioural and Emotional Challenges
Living with a long-term neurological condition like dystonia can impact emotional well-being. It may contribute to behavioural and psycho-emotional challenges such as anxiety, depression, or social interaction difficulties.
Several studies of children and adults with movement disorders have shown that high proportion of patients had anxiety, depression, or mixed mental health disorders.
How to diagnose Movement Disorders or Dystonia?
Diagnosing movement disorder in children involves a thorough evaluation by a paediatric neurologist, including medical history, physical examination, developmental assessment, and neurological evaluation.
During your appointment, Dr Yeo will want to know as much as possible about the nature of the abnormal movement.
It will help Dr Yeo by providing the following information:
- Diary of your child’s event or abnormal movement (dates, times, description of what had happened before/during/ after the event)
- Video recording of your child’s abnormal movement (if possible)
- Bring along the individual who had witnessed your child’s event or get a written description from the individual who had witnessed your child’s event would be very helpful!
Dr Yeo may suggest the following tests to help with the diagnosis and management of the abnormal movement or movement disorder:
- Electroencephalogram (EEG) : This is a brain-wave recording which involves applying quite a few sticky sensors on your child’s head. This is a painless procedure.
- Magnetic Resonance Imaging (MRI) of the brain: These are detailed pictures of the brain to evaluate the structure of your child’s brain.
- Comprehensive neurometabolic testing and/ or genetic testing may be offered to identify underlying metabolic or genetic causes.
Early diagnosis and appropriate treatments are crucial for optimising long term neuro-developmental outcomes and providing appropriate support for children with dystonia or other movement disorders and their families.
How do we treat Movement Disorder?
Once your child is diagnosed with a movement disorder, Dr. Yeo will work with you to create a personalised treatment plan. This plan will consider all aspects of your child’s lifestyle and situation and your family’s preferences.
Dr Yeo may also collaborate with you and your child to create a Dystonia Action Plan, which is an emergency plan to follow when an intrusive dystonia occurs. This plan will include vital information about your child’s medical history, dystonia/ movement disorders, and regular and emergency medication plans.
After considering all of these aspects, Dr. Yeo will guide you and your child in finding the proper treatment; There are a number of different treatments that can reduce the symptoms of dystonia and other movement disorders:
Oral Medication
Specific medications for managing dystonia, spasticity and movement disorders are available. These medications aim to modulate or stabilize abnormal electrical signals in brain cells or restore chemical imbalances.
In addition, other medications may be prescribed to address symptoms associated with movement disorders, such as pain, muscle stiffness (spasticity), seizures, or gastrointestinal issues. Common options include muscle relaxants, anti-seizure medications, pain relievers, and medications for reflux or constipation.
Dr. Yeo will discuss which medications have been effective for your child’s specific movement disorder and outline the advantages and disadvantages, such as side effects of each treatment option.
Pharmacomodulation Therapy
Pharmacomodulation therapy offers an effective solution for effectively reducing muscle spasticity and dystonia. By enhancing the range of motion and maintaining optimal joint alignment, this therapy significantly improves overall comfort and quality of care. When combined with physical and/or occupational therapy, serial casting, oral therapy and orthotic devices, it not only facilitates essential stretching exercises but also supports standing and functional activities.
Please click here for additional information about pharmacomodulation therapy.
Physical Therapy
Physical therapy focuses on improving muscle strength, flexibility, balance, posture and mobility through exercises and specific therapeutic techniques for tackling movement disorders. It may also include training in activities of daily living and the use of assistive devices such as braces or walkers.
Occupational Therapy
Occupational therapy helps individuals develop skills for daily tasks, such as dressing, feeding, and writing, to promote independence and improve quality of life. It may involve adaptive equipment and techniques tailored to the individual’s needs.
Speech Therapy
Speech therapy addresses communication difficulties, swallowing problems (dysphagia), and oral motor issues commonly associated with movement disorders. Therapists work to improve speech clarity, language skills, and swallowing function.
There are other treatment options which may be suggested if they are appropriate:
Intrathecal Infusion Therapy
Generalised dystonia or spasticity can be treated with physiotherapy and oral medications, but these are sometimes ineffective or have unacceptable side effects due to high dosage. Intrathecal infusion therapy involves injecting medication into the cerebrospinal fluid which surrounds the spinal cord. A pump implanted in the abdomen injects into the cerebrospinal fluid, increasing the drug’s effectiveness and reducing adverse events.
Intrathecal infusion therapy has demonstrated a dramatic improvement in severe generalised dystonia/ spasticity together with long-term safety.
Deep Brain Stimulation (DBS)
Deep brain stimulation (DBS) is an advanced functional neurosurgical procedure designed to transform the lives of individuals affected by debilitating movement disorders. This advanced technique involves the precise implantation of two thin electrodes into the brain, which are then connected by a wire that runs under the skin to a battery, typically placed in the chest or abdomen. Acting much like a pacemaker, the battery delivers targeted electrical pulses that significantly modulate the brain’s signals responsible for conditions such as dystonia, tremors, and myoclonus.
Non-invasive Neuromodulation Therapy
Non-invasive neuromodulation techniques, including Transcranial Pulsed Current Stimulation (tPCS) and Transcutaneous Electrical Nerve Stimulation (TENS), represent a revolutionary approach to treating neurological diseases. By effectively modulating neuronal signals without the need for invasive procedures, these cutting-edge methods tap into the brain’s remarkable ability to adapt and reorganise, known as neuroplasticity. This empowers patients with safe and impactful treatment options.
If you have any further questions, you can schedule an appointment today with Dr Yeo.
References
Dr Yeo’s recent peer-group review journal publications and relevant articles regarding Cerebral Palsy (CP) and Long Term Neurological Conditions (LTNC):
Weller, L.J.R., Sherwood, S.-A.M., Ng, S.H., Vellaichamy, M., Noordin, A.A., Tan, L.Y., Mahadev, A., Yeo, T.H. and Ng, Z.M. (2025), Can External Neuromodulation Garments Improve Gait and Function in Children With Cerebral Palsy? A Prospective Single-Arm Study. Health Science Reports, 8: e70566. https://doi.org/10.1002/hsr2.70566
Cheng, Duo-Tong, Yeo, Tong Hong, Seng, Michaela Su-Fern, Teoh, Oon Hoe, Lee, Sumin; Koh, Ai Ling. Genomic sequencing: ending the diagnostic odyssey for a child with microcephaly and dystonia with a perioperative challenge. Singapore Medical Journal ():10.4103/singaporemedj.SMJ-2023-134, June 28, 2024. | DOI: 10.4103/singaporemedj.SMJ-2023-134
Chia, Aletheia & Tan, Yi & Yeo, Tong & Teoh, Oon & Ng, Zhi Min. (2022). Epidemiology and risk factors for sleep disturbances in children and youth with cerebral palsy: An ICF-based approach. Sleep Medicine. 96. 10.1016/j.sleep.2022.04.021.
Leow, XYJ & Tan, JTC & Yeo, Tong & Wong, Kenneth & Mahadev, Arjandas & Ang, Bixia & Vasanwala, Rashida & Ng, Zhi Min. (2021). Evaluation of risk factors associated with fragility fractures and recommendations to optimise bone health in children with long-term neurological condition. Singapore Medical Journal. 64. 10.11622/smedj.2021124.
Ng, Zhi Min & Lin, Jeremy & Khoo, Poh & Rajadurai, Victor & Chan, Derrick & Ong, Hian & Wong, Janice & Choong, Chew & Lim, Kim & Lim, Kevin & Yeo, Tong. (2021). Causes, functional outcomes and healthcare utilisation of people with cerebral palsy in Singapore. Annals of the Academy of Medicine, Singapore. 50. 111-118. 10.47102/annals-acadmedsg.2020489.
KKH Hip Surveillance Programme for Children with Long term Neurological Conditions
Special Delivery, Issue 3, March 2018
(By Dr Ng Zhi MIn, Dr Yeo Tong Hong, A/Prof Arjandas Mahadev)
Yeo TH, Brooks L, Differences in perceptions of palliative care needs for children with neurological conditions. Support Palliat Care 2012;2:A18.
Research
- Co-investigator, Singapore Cerebral Palsy Registry, 2017 – ongoing research project
- Local principal investigator, Royal Hospital for Children, Glasgow, UKMCRN trial – ‘The efficacy, safety and tolerability of nabiximols as an adjunctive treatment to existing anti-spasticity medications in children aged 8 to 18 years with spasticity due to cerebral palsy who have not responded adequately to their existing anti-spasticity medications: a parallel group randomised, double-blind, placebo-controlled study’, 2014 – 2016.