What is Hypotonia?
- ‘Decreased resistance to passive movement’ or ‘low muscle tone’
- Usually associated with joint hyper mobility
- May be associated with reduction in spontaneous movement
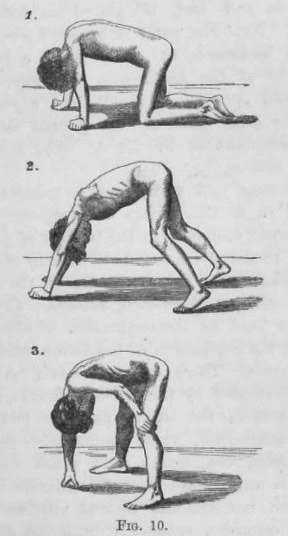

(Figure depicting a child with positive Gower sign)
(Picture of a floppy baby)
What are the causes of hypotonia?
There are many reasons why an infant may be hypotonic. With a structured approach, including experienced assessment and personalised investigations, a Paediatric Neurologist can differentiate the following causes.
Central Causes:
- Primary Neurological Abnormality, e.g. malformation of brain, Prader Willi Syndrome
- Due to disordered function elsewhere, e.g. heart condition, metabolic disorder
Peripheral Causes:
- Anterior Horn Cell causes, e.g. Spinal Muscular Atrophy (SMA)
- Lower motor neuron or peripheral nerve issues, e.g. Axonal Neuropathy
- Neuromuscular junction issues, e.g. Myasthenia
- Muscle causes, e.g. Myopathy
Mixed:
- Both central and peripheral causes, e.g. Mitochondrial disorder, Congenital Muscular Dystrophy
When shall I see a Paediatric Neurologist?
- Identifying the Underlying Cause: It is essential to determine the root cause of hypotonia to ensure that significant neuromuscular or genetic disorders are not missed.
- Personalized Diagnostic Approach: We strive to tailor specific diagnostic tests when necessary, reducing the likelihood of unnecessary investigations and focusing on what truly matters for your child’s health.
- Informed Management Decisions: Our evaluation will guide decisions about management strategies and possible targeted treatments, empowering you with actionable insights.
- Accurate Prognosis and Risk Assessment: We provide clear prognostic information and assess the risk of recurrence as well as options for future antenatal testing.
During your appointment, Dr. Yeo will conduct a comprehensive evaluation, including an in-depth medical history, a thorough physical examination, and an extensive neurological assessment.
Following this careful evaluation, Dr. Yeo may recommend further investigations to get a clearer picture of your child’s condition. These tests may include blood, urine, or cerebrospinal fluid (CSF) analysis to measure specific chemical or mineral levels, along with audiological and ophthalmological evaluations. If indicated, MRI of the brain is advised, given its superior ability to detect subtle abnormal changes. Additionally, electromyography (EMG) and nerve conduction studies (NCS) may be utilised to analyse your child’s muscle and nerve signals. Depending on the findings from the initial assessment, we may also recommend genetic testing or a muscle biopsy to provide further clarity.
You can trust that our approach is thorough, thoughtful, and focused on achieving the best possible outcomes for your child’s health.
Please click ‘Blood Tests & Metabolic Testing’ and ‘Genetic Testing’ for details.
If you have any further questions, you can schedule an appointment today with Dr Yeo.
References
Dr Yeo’s recent peer-group review journal publications and abstracts regarding Neurometabolic disorders:
Leow, XYJ & Tan, JTC & Yeo, Tong & Wong, Kenneth & Mahadev, Arjandas & Ang, Bixia & Vasanwala, Rashida & Ng, Zhi Min. (2021). Evaluation of risk factors associated with fragility fractures and recommendations to optimise bone health in children with long-term neurological condition. Singapore Medical Journal. 64. 10.11622/smedj.2021124.
Hamilton R, Yeo TH, et al. Sensitivity and specificity of the light-adapted ERG in suspected neuronal ceroid lipofuscinoses (NCLs). Documenta Ophthalmologica, Aug 2016;133 (1S).
Yeo TH, Vassallo G, Judge M, Laycock N, Kelsey A, Crow YJ. Infantile neurological Degos disease. Eur J Paediatr Neurol. 2011 Mar;15(2):167-70.
Yeo TH, De Goede C, Crow Y. Biotin non-responsive familial infantile bilateral striatal necrosis associated with primary Influenzae A infection. Eur J Paediatr Neurol. 2011 May:15(1):S117-S118.
Yeo TH, et al. Coexistence of Krabbe’s disease and multiple chromosomal abnormalities: a case report. Poster presentation. Eur J Paediatr Neurol. Eur J Paediatr Neurol. 2011 May:15(1): S52-S53.
Yeo TH, et al. The value of CT brain in undiagnosed neurological disorders. Eur J Paediatr Neurol. 2009 Sept: 13(1):S124.