Cerebral palsy is an umbrella term for a group of permanent disorders that affect movement and/or posture and motor function. It is one of the most common and severe disabilities in childhood.
What is Cerebral Palsy?
CP affects the brain’s ability to control muscles. It is caused by an injury to a developing brain that regulates movement, balance, and posture. This injury can occur during pregnancy, childbirth, or early childhood. The severity of CP varies and can impact muscle tone, coordination, and motor functions. While CP does not worsen over time, the symptoms may change as a child grows. Additionally, CP can coexist with other conditions, such as epilepsy or learning disabilities. Treatment focuses on improving mobility, managing symptoms, and supporting the child’s development.
What causes Cerebral Palsy?
CP is caused by abnormal brain development or injury to the developing brain, particularly in areas that control movement, balance, and posture. The exact cause of CP can vary and may not always be identified. However, several factors can contribute to its development:
Before Birth:
- Abnormal brain development during pregnancy can result from genetic disorders, infections, maternal health conditions, or exposure to toxins or radiation.
- Infections during pregnancy, such as rubella (German measles), cytomegalovirus (CMV), or toxoplasmosis, can increase the risk of CP.
- Certain maternal health conditions, such as thyroid disorders or diabetes, can affect fetal brain development and raise the risk of CP.
During Delivery:
- Oxygen deprivation or trauma during labor and delivery – due to complications such as umbilical cord issues, placental abruption, or prolonged labour can lead to brain damage and result in CP.
- Premature infants are at a higher risk for CP due to their vulnerable and underdeveloped brains and blood vessels.
Postnatal Period:
- Traumatic brain injuries, infections (like meningitis or encephalitis), or other acute neurological conditions occurring after birth can lead to CP.
- A stroke in infants or young children can cause brain damage, resulting in CP.
- Untreated severe jaundice (hyperbilirubinaemia) in newborns can result in a type of brain damage known as kernicterus, which can lead to dyskinetic CP.
What Are the Types of Cerebral Palsy?
Cerebral Palsy (CP) encompasses several different types, each characterised by specific movement and coordination issues. The primary types of CP are as follows:
1. Spastic Cerebral Palsy
This is the most common type, affecting approximately 70% of individuals with CP. It causes stiffness and tightness in the muscles, leading to difficulties with movement and range of motion. The subtypes of spastic cerebral palsy include:
- Spastic Hemiplegia: One side of the body is affected, with the arm usually being more impacted than the leg.
- Spastic Diplegia: Both legs are more affected than the arms.
- Spastic Quadriplegia: All four limbs are affected, often with severe involvement of both arms and legs.
2. Dyskinetic Cerebral Palsy
This type includes dystonic, athetoid, or choreoathetoid forms. It involves involuntary movements such as twisting, writhing, or jerking motions. Individuals may have difficulty controlling their posture and may experience fluctuations in muscle tone, alternating between stiffness and floppiness. Children with dyskinetic CP may receive an incorrect initial diagnosis. Therefore, all children who present with early onset dystonia or dyskinesia should be assessed by a paediatric neurologist.
3. Mixed Cerebral Palsy
Some individuals with CP may exhibit symptoms that do not fit neatly into one category but show characteristics of multiple types. For example, a person may display both spasticity and dyskinesia.
4. Ataxic Cerebral Palsy
Ataxia refers to poor balance and lack of coordination. The definition and description of ataxic CP are generally lacking, and a high proportion of individuals with ataxic CP may receive an incorrect initial diagnosis. Therefore, all children who present with early onset ataxia or ataxic CP should be assessed by a paediatric neurologist.
5. Hypotonic Cerebral Palsy
Hypotonic means low muscle tone. A significant number of individuals with hypotonic CP may also receive an incorrect initial diagnosis. All children exhibiting axial or peripheral hypotonia or hypotonic CP should be evaluated by a paediatric neurologist.
What Are the Signs and Symptoms of Cerebral Palsy?
Cerebral Palsy (CP) can present with a variety of signs and symptoms, which may vary in severity and combination from one individual to another. Some common signs and symptoms of CP include:
Developmental Delay
- Delays in reaching developmental milestones such as sitting up, crawling, walking, or speaking.
- Difficulty with fine motor skills like grasping objects or holding a utensil.
Motor Disorder and/or Movement Disorder
- Spasticity – Muscle stiffness or tightness
- Dystonia – Involuntary muscle spasms, repetitive awkward and twisting posture
- Athetosis – Involuntary slow, flowing, writhing, worm-like movement
- Chorea – Involuntary rapid, irregular, excessive, dance-like movement
- Ballimus – Involuntary rapid, violent flinging movement
Abnormal Deep Tendon Reflexes
- Persistent primitive reflexes beyond infancy, such as the Moro reflex (startle reflex) or Asymmetric Tonic Neck Reflex (ATNR).
- Exaggerated deep tendon reflexes in response to stimuli or tendon hammer.
Poor Balance & Coordination
- Fidgety, jerky or clumsy movement
- Random, uncontrolled movement
Gait & Mobility impairment
- Scissoring – Legs cross or “scissor” when walking due to tight muscles (dystonia)
- Toe walking – Walking on tiptoes instead of using a typical heel-to-toe pattern.
Speech & Swallowing impairment
- Dysarthria – Difficulty with articulation and control of speech muscles, leading to slurred or unclear speech.
- Dysphagia – Difficulty with swallowing, which may result in choking or aspiration.
Other Symptoms
- Seizures & Epilepsy – 25% of children with CP may experience epileptic seizures, which can vary in type and severity.
- Learning Disabilities – While CP primarily affects movement and posture, some individuals may also have cognitive impairments or learning disabilities.
What are other associated conditions?
Individuals with Cerebral Palsy (CP) may experience a variety of co-occurring conditions that can impact their overall health and well-being. Some common co-occurring conditions include:
Cognitive impairment
While CP primarily affects movement and posture, 25% of children with CP may also have learning disabilities or cognitive impairments that affect learning, problem-solving, and adaptive functioning.
Epilepsy and Epileptic Seizures
25% of children with CP may experience seizures. These seizures can vary in type and severity and may require treatment with anti-seizure medications.
Speech and Communication difficulties
CP can affect the muscles involved in speech and communication, leading to difficulties with articulation, clarity, and fluency in up to 40% of children with CP. Speech and language therapy may be beneficial in improving communication skills.
Vision Impairment
40% of children with CP have visual impairments, which may include strabismus (crossed eyes), nystagmus (involuntary eye movements), or cortical visual impairment. Regular ophthalmological assessment and interventions may be necessary.
Hearing Impairment
9% of children with CP may also experience hearing impairments, either due to congenital factors, complications of prematurity, or repeated ear infections. Hearing assessment and appropriate interventions are essential for optimal communication and development.
Gastrointestinal Issues
Digestive problems such as gastroesophageal reflux disease (GERD), constipation, or difficulty swallowing (dysphagia) are common in individuals with CP. Proper management and dietary modifications may be necessary to address these issues.
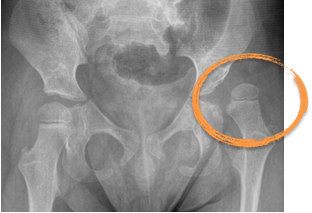
Orthopaedic Complications
Up to 20% of children with CP can lead to musculoskeletal issues such as hip subluxation/ dislocation, scoliosis,and joint deformities due to muscle stiffness or muscle weakness. Physical therapy, pharmacological treatments, orthotic devices or surgical interventions may be required to manage these complications.
Behavioural and Emotional Challenges
Living with a long term neurological condition like CP can impact emotional well-being and may contribute to behavioural and psycho-emotional challenges such as anxiety, depression, or social interaction difficulties. Counselling and psychosocial support can help address these issues.
Dental and Oral Health Problems
Individuals with CP may be at increased risk of dental caries, gum disease, or malocclusion (misalignment of teeth) due to factors such as poor oral hygiene, difficulty with oral care, or dental anomalies.
Sleep Disorders
Sleep disturbances such as sleep apnea, insomnia, or disrupted sleep patterns are more prevalent in children with CP (up to 15-20%) and may affect overall health and quality of life.
How to diagnose Cerebral Palsy?
Diagnosing Cerebral Palsy (CP) in children involves a thorough evaluation by paediatric neurologist, including medical history, physical examination, developmental assessment, and neurological evaluation. Diagnostic criteria based on clinical signs of motor impairments, abnormal muscle tone, and non-progressive motor dysfunction confirm the diagnosis.
Collaboration with multidisciplinary teams, including therapists and specialists, helps assess functional abilities and rule out other conditions. Family history and genetic testing may be considered to identify underlying genetic factors. Early detection and intervention are crucial for optimising outcomes and providing appropriate support for children with CP and their families.
What Are The Treatment Options For Cerebral Palsy?
Treatment options for Cerebral Palsy (CP) aim to manage symptoms, improve mobility and function, and enhance overall quality of life for individuals affected by the condition. Here are common treatment approaches:
Physiotherapy
Physical therapy focuses on improving muscle strength, flexibility, balance, and mobility through exercises and therapeutic techniques. It may also include training in activities of daily living and the use of assistive devices such as braces or walkers.
Physiotherapist may use Functional Electrical Stimulation (FES) as part of therapy programme; it involves applying electrical stimulation to muscles to improve muscle strength, reduce spasticity, and promote functional movement, particularly in individuals with weak or paralysed muscles.
Occupational Therapy
Occupational therapy helps individuals develop skills for daily tasks, such as dressing, feeding, and writing, to promote independence and improve quality of life. It may involve adaptive equipment and techniques tailored to the individual’s needs.
Speech & Language Therapy
Speech therapy addresses communication difficulties, swallowing problems (dysphagia), and oral motor issues commonly associated with CP. Therapists work to improve speech clarity, language skills, and swallowing function.
Medications
Medications may be prescribed to manage symptoms associated with CP, such as spasticity/ dystonia, seizures, pain, or gastrointestinal issues. Common medications include muscle relaxants, brain cell modulators, anti-seizure medications, pain relievers, and medications for reflux or constipation.
Pharmacomodulation Therapy
Pharmacomodulation therapy temporarily reduces muscle spasticity or dystonia, and it aims to improve the range of motion, preserve joint alignment, and to improve ease of comfort and care. They are commonly used in conjunction with physical and/or occupational therapy, serial casting and orthotic devices to facilitate stretching exercises, standing and functional activities.
Non-invasive Neuromodulation Therapy
Non-invasive neuromodulation techniques, including Transcranial Pulsed Current Stimulation (tPCS) and Transcutaneous Electrical Nerve Stimulation (TENS), represent a revolutionary approach to treating neurological diseases. By effectively modulating neuronal signals without the need for invasive procedures, these cutting-edge methods tap into the brain’s remarkable ability to adapt and reorganise, known as neuroplasticity. This empowers patients with safe and impactful treatment options.
Intrathecal Infusion Therapy
Spasticity can be treated with physiotherapy and oral medications but these are sometimes ineffective or have unacceptable side effects. Intrathecal treatment involves injecting medication into the cerebrospinal fluid which surrounds the spinal cord. A pump implanted in the abdomen injects into the cerebrospinal fluid, increasing the drug’s effectiveness and reducing adverse events.
Intrathecal infusion therapy therapy has demonstrated a dramatic improvement in severe spasticity together with long-term safety.
Orthopaedic Interventions
Orthopaedic treatments may be necessary to address functional musculoskeletal deformities such as hip subluxation/ dislocation, contractures, scoliosis, or joint deformities.
Selective Dorsal Rhizotomy (SDR)
SDR is a neurosurgical procedure that involves cutting specific nerves in the spinal cord to reduce spasticity and improve mobility in selected children with CP.
Alternative and Complementary Therapies
Alternative therapies, such as hippotherapy (horseback riding), aquatic therapy, acupuncture, or massage, may complement conventional treatments and promote relaxation, pain relief, and improved mobility.
If you have any further questions, you can schedule an appointment today with Dr Yeo.
References
Dr Yeo’s recent peer-group review journal publications and relevant articles regarding Cerebral Palsy (CP) and Long Term Neurological Conditions (LTNC):
Weller, L.J.R., Sherwood, S.-A.M., Ng, S.H., Vellaichamy, M., Noordin, A.A., Tan, L.Y., Mahadev, A., Yeo, T.H. and Ng, Z.M. (2025), Can External Neuromodulation Garments Improve Gait and Function in Children With Cerebral Palsy? A Prospective Single-Arm Study. Health Science Reports, 8: e70566. https://doi.org/10.1002/hsr2.70566
Cheng, Duo-Tong, Yeo, Tong Hong, Seng, Michaela Su-Fern, Teoh, Oon Hoe, Lee, Sumin; Koh, Ai Ling. Genomic sequencing: ending the diagnostic odyssey for a child with microcephaly and dystonia with a perioperative challenge. Singapore Medical Journal ():10.4103/singaporemedj.SMJ-2023-134, June 28, 2024. | DOI: 10.4103/singaporemedj.SMJ-2023-134
Chia, Aletheia & Tan, Yi & Yeo, Tong & Teoh, Oon & Ng, Zhi Min. (2022). Epidemiology and risk factors for sleep disturbances in children and youth with cerebral palsy: An ICF-based approach. Sleep Medicine. 96. 10.1016/j.sleep.2022.04.021.
Leow, XYJ & Tan, JTC & Yeo, Tong & Wong, Kenneth & Mahadev, Arjandas & Ang, Bixia & Vasanwala, Rashida & Ng, Zhi Min. (2021). Evaluation of risk factors associated with fragility fractures and recommendations to optimise bone health in children with long-term neurological condition. Singapore Medical Journal. 64. 10.11622/smedj.2021124.
Ng, Zhi Min & Lin, Jeremy & Khoo, Poh & Rajadurai, Victor & Chan, Derrick & Ong, Hian & Wong, Janice & Choong, Chew & Lim, Kim & Lim, Kevin & Yeo, Tong. (2021). Causes, functional outcomes and healthcare utilisation of people with cerebral palsy in Singapore. Annals of the Academy of Medicine, Singapore. 50. 111-118. 10.47102/annals-acadmedsg.2020489.
KKH Hip Surveillance Programme for Children with Long term Neurological Conditions
Special Delivery, Issue 3, March 2018
(By Dr Ng Zhi MIn, Dr Yeo Tong Hong, A/Prof Arjandas Mahadev)
https://www.kkh.com.sg/about-kkh/newsroom/publications/Documents
Special_Delivery_Issue_3_2018.pdf
Yeo TH, Brooks L, Differences in perceptions of palliative care needs for children with neurological conditions. Support Palliat Care 2012;2:A18.
Research Trials
- Co-investigator, Singapore Cerebral Palsy Registry, 2017 – ongoing research project
- Local principal investigator, Royal Hospital for Children, Glasgow, UKMCRN trial – ‘The efficacy, safety and tolerability of nabiximols as an adjunctive treatment to existing anti-spasticity medications in children aged 8 to 18 years with spasticity due to cerebral palsy who have not responded adequately to their existing anti-spasticity medications: a parallel group randomised, double-blind, placebo-controlled study’, 2014 – 2016.